
Advanced 1.5T Extremity MR Imaging Assisting Research of Cartilage Regeneration Using Stem Cells

[clear_flat]
Since its establishment in 2005, KLSMC has attracted patients and medical referrals from around the world. Arthroscopic and joint replacement surgeries are routinely performed at the hospital.
In May, 2011, the hospital’s dedicated Sports Imaging department began utilizing GE Healthcare’s 1.5T ONI MSK Extremity MR. As a direct result of this implementation, workflow was streamlined; resulting in an increased number of patients and a higher-quality MRI has enhanced the standard of care. The high field extremity MR scanner was also pivotal to a clinical trial conducted at KLSMC that is focusing on the utilization of stem cell therapy for treating damaged knee cartilage.
[divider]
Stem cell research on cartilage regeneration
Degenerative changes to the joints occur when there is a breakdown of articular cartilage. Cartilage regeneration using the patient’s own stem cells has made the treatment of complex cartilage injuries possible, especially at the knee.
According to Khay-Yong Saw, founder and senior partner of KLSMC, stem cells in adults act as a repair system for the body, allowing replacement of ageing and damaged cells in organs. “In adults, damaged tissue is usually replaced with scar tissue which loses most of its original function. Stem cell therapy has the potential to restore the original structure and function of the damaged tissue.”
A 2011 study co-authored by Dr. Saw and his colleagues at KLSMC showed that it was possible to regenerate a better cartilage by injecting a combination of peripheral blood stem cells (PBSC) and hyaluronic acid (HA) into the defective areas following subchondral drillings.1
And, in showing that post-operative intra-articular injections of autologous PBSC with HA resulted in improvement in the quality of repair cartilage over the same treatment without stem cells,2 the GE 1.5T ONI MSK Extremity MR was used to assess all post-operative repair cartilage.
Typically, harvesting is performed one week after arthroscopic subchondral drilling of the chondral lesions. To enable harvesting, a dual lumen catheter is inserted into the femoral vein. The catheter allows blood to be passed through a cell separator which filters out stem cells and returns the processed blood to the body. This procedure is called apheresis. The stem cells are prompted to move into the bloodstream using a hormone called G-CSF, a hormone produced by the body that stimulates the production of marrow stem cells which enter the bloodstream. A local anesthetic is used to minimize discomfort from the venous cannulation which is performed under ultrasound guidance. Once harvesting is complete, the catheter is removed and the stem cells can be used immediately for treatment or be cryopreserved for use at a later date.
Interval MR exams by 1.5T ONI MSK Extremity MR has shown satisfactory healing of the chondral defects including the subchondral bone. The MR images also clearly showed evidence of cartilage regeneration. This newfound innovative procedure is not limited to small isolated lesions but can be used to treat large, multi-compartment lesions, including “kissing lesions.”
Perhaps more importantly for patients, the surgery is a single stage arthroscopic procedure followed by subsequent intra-articular injections of PBSC and HA. There is no second surgery or open surgery required, as in the case of other cartilage repair techniques. Stem cell therapy can also be extended to ligaments, muscles, and bone injuries, attesting to the pluripotential properties of PBSC.3 Dr. Saw has treated some of the country’s top athletes and weekend warriors alike with this cartilage regeneration technique.
[divider]
Arthroscopic images
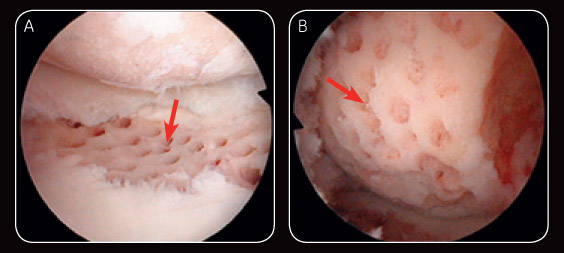
Fig. 1 Arthroscopic image illustrating post-subchondral drilling over the lateral tibial plateau (A) and post-subchondral drilling of the lateral femoral condyle (B).
Post-operative MR
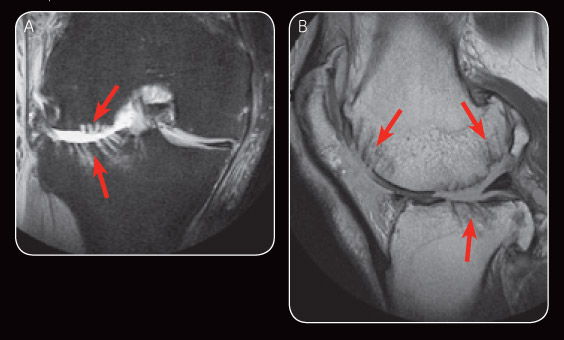
Fig. 2 Early post-operative MR images: PDFS (A) illustrates subchondral drilling at the lateral femoral condyle and lateral tibial plateau. Sagital PD (B) shows areas of subchondral drilling.
Six-month follow-up
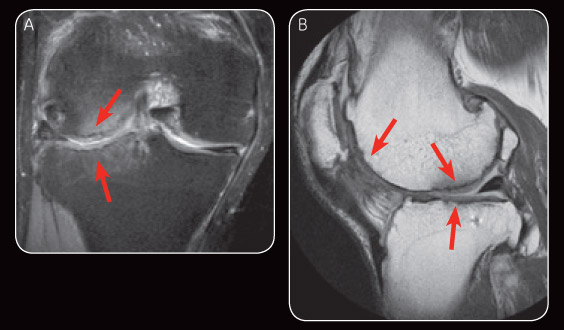
Fig. 3 Appearance on MR image at six-month follow-up demonstrates satisfactory repair cartilage and minimal subchondral oedema (A). Sagital PD at six-month follow-up also demonstrates satisfactory repair cartilage (B).
The use of a high field extremity MR scanner is the key in enabling us to better visualize the repair cartilage.
Dr. Khay-Yong Saw
[divider]
Optimized workflow and improved clinical care
In addition to playing an important role in the stem cell research and cartilage regeneration at KLSMC, the dedicated 1.5T system provides KLSMC with an improved workflow, flexibility, and reliable anatomy-specific imaging capabilities. As a significant portion of the caseload at KLSMC involves the extremities, the system was the natural choice to facilitate MR imaging, not just of the knees, ankles, wrists, and elbows.
“Since implementing the GE 1.5T extremity system, we are now able to conduct examinations on very specific cases of sports-related injuries,” says Dr. Shahrin Merican, consultant radiologist at KLSMC.
Besides being able to handle a greater caseload, the system has also helped reduce patients’ waiting time and allow same-day imaging to be performed at KLSMC. “Approximately 25% of our patients come from other parts of Malaysia and overseas, and our ability to provide same-day imaging at the first clinic visit is a significant convenience for them,” says Dr. Merican. “Same-day imaging provides earlier diagnosis and allows prompt formulation of a treatment plan.”
This increased level of patient volume has improved productivity and increased the economic benefit. The system provides high-quality imaging at a fraction of the price of conventional whole body MR scanners. The compact system has a much smaller footprint, taking up less floor space and uses less electricity for significant cost savings.
Dr. Merican adds, “What’s also important from a clinical care perspective, is the patients’ level of comfort and ease-of-mind when undergoing their MR scans. We find that our patients have been impressed by the small size and quiet operation of the scanner. Patients are much less intimidated by the machine, and claustrophobia is rarely an issue.”
The implementation of the system has ultimately contributed to a more conducive clinical and research environment at KLSMC. Dr. Saw explains the installation of the extremity scanner shows promising results for the assessment of cartilage regeneration. “The use of a high-field extremity MR scanner is the key in enabling us to better visualize the repair cartilage,” he says. Regarding clinical use of the 1.5T extremity scanner, Dr. Merican adds, “By allowing us to make confident diagnoses through the use of a reliable, patient-friendly scanner, we expect to gain from an increase in the number of medical referrals resulting directly from the greater patient satisfaction that has been achieved.”
[divider]
References
- Saw KY, Anz A, Merican S, et al. Articular Cartilage Regeneration With Autologous Peripheral Blood Progenitor Cells and Hyaluronic Acid After Arthroscopic Subchondral Drilling: A Report of 5 Cases With Histology. The Journal of Arthroscopy and Related Surgery, April 2011. Vol 27, No 4:493-506.
- Saw KY, Anz A, Jee CSY, Merican S, et al. Articular Cartilage Regeneration With Autologous Peripheral Blood Stem Cells Versus Hyaluronic Acid: Randomized Controlled Trial. The Journal of Arthroscopy and Related Surgery, April 2013. Vol 29, No 4:684-694.
- K-Y.Saw, C.S-Y.Jee. From Blade Runner to Stem-Cell Player and Beyond. Bone & Joint 360, Volume 2, Issue 1, February 2013.
Source: GE Signa Pulse Spring 2013 ISMRM
Download Article Leave a reply