Publications
Saw, K. Y., Jee, C. S. Y., Dawam, A., Ramlan, A., & Anz, A. W., (2022). Stem Cell Therapy Brings New Life to Musculoskeletal Regeneration. Research Outreach, 132. DOI: 10.32907/RO-132-3316289888
Saw, K. Y., Anz, A. W., Jee, C. S. Y., Low, S. F., Dawam, A., & Ramlan, A. (2023). Osteochondral Regeneration in the Knee Joint with Autologous Peripheral Blood Stem Cells plus Hyaluronic Acid after Arthroscopic Subchondral Drilling: Report of Five Cases. Orthopaedic Surgery. DOI: 10.1111/os.13949
Saw, K. Y., Jee, C. S. Y., Ramlan, A., Dawam, A., Saw, Y. C., & Low, S. F. (2022). Osteochondrogenesis with Autologous Peripheral Blood Stem Cells for Osteochondral Lesions of the Talus: Report of Five Cases. Malaysian orthopaedic journal, 16(3), pp: 128 – 131. DOI: 10.5704/MOJ.2211.019
Saw, K. Y., Anz, A. W., Ng, R.C.S., & Jee, C. S. Y., (2021). Stem Cell-Based Cartilage Regeneration Technology. Research Outreach, 127. DOI: 10.32907/RO-127- 1985367964
Saw, K. Y., Low, S. F., Ramlan, A., Dawam, A., Saw, Y. C., & Jee, C. S. Y. (2022). Autologous Peripheral Blood Stem Cell Therapy for Chronic Achilles Tendinopathy: Report of Three Cases. Malaysian Orthopaedic Journal, 16(2), pp 150 – 154. DOI: 10.5704/MOJ.2207.022
Saw KY, Anz AW, Jee CSY, Ramlan A, Dawam A, Low SF. Chondrogenesis with Autologous Peripheral Blood Stem Cells for End-Stage Ankle Arthritis: Report of Three Cases. Malays Orthop J. 2022; 16(1): 134-7. doi: 10.5704/MOJ.2203.022
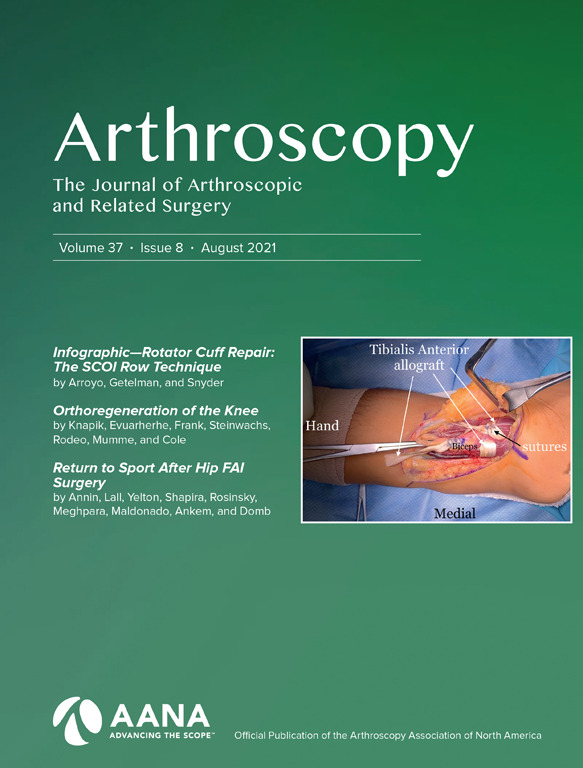
Arthroscopic Subchondral Drilling Followed by Injection of Peripheral Blood Stem Cells and Hyaluronic Acid Showed Improved Outcome Compared to Hyaluronic Acid and Physiotherapy for Massive Knee Chondral Defects: A Randomized Controlled Trial
Arthroscopy: The Journal of Arthroscopic and Related Surgery, Vol 37, No 8 (August), 2021: pp 2502-2517. By Khay-Yong Saw, Adam W. Anz, Reza Ching-Soong Ng, Caroline Siew-Yoke Jee, Soo Fin Low, Christopher Dorvault, Kevin B. Johnson.
Purpose
The purpose of this study was to evaluate the safety and efficacy of intra-articular injections of autologous peripheral blood stem cells (PBSCs) plus hyaluronic acid (HA) after arthroscopic subchondral drilling into massive chondral defects of the knee joint and to determine whether PBSC therapy can improve functional outcome and reduce pain of the knee joint better than HA plus physiotherapy.
Methods
This is a dual-center randomized controlled trial (RCT). Sixty-nine patients aged 18 to 55 years with International Cartilage Repair Society grade 3 and 4 chondral lesions (size ≥3 cm2) of the knee joint were randomized equally into (1) a control group receiving intra-articular injections of HA plus physiotherapy and (2) an intervention group receiving arthroscopic subchondral drilling into chondral defects and postoperative intra-articular injections of PBSCs plus HA. The coprimary efficacy endpoints were subjective International Knee Documentation Committee (IKDC) and Knee Injury and Osteoarthritis Outcome Score (KOOS)–pain subdomain measured at month 24. The secondary efficacy endpoints included all other KOOS subdomains, Numeric Rating Scale (NRS), and Magnetic Resonance Observation of Cartilage Repair Tissue (MOCART) scores.
Results
At 24 months, the mean IKDC scores for the control and intervention groups were 48.1 and 65.6, respectively (P < .0001). The mean for KOOS-pain subdomain scores were 59.0 (control) and 86.0 (intervention) with P < .0001. All other KOOS subdomain, NRS, and MOCART scores were statistically significant (P < .0001) at month 24. Moreover, for the intervention group, 70.8% of patients had IKDC and KOOS-pain subdomain scores exceeding the minimal clinically important difference values, indicating clinical significance. There were no notable adverse events that were unexpected and related to the study drug or procedures.
Conclusions
Arthroscopic marrow stimulation with subchondral drilling into massive chondral defects of the knee joint followed by postoperative intra-articular injections of autologous PBSCs plus HA is safe and showed a significant improvement of clinical and radiologic scores compared with HA plus physiotherapy.
Level of Evidence
Level I, RCT.
Editorial Commentary: Peripheral Blood Stem Cells Mobilization Using Granulocyte Colony-Stimulating Factor for Articular Cartilage Injuries: Wake Them Up and Make Them Come to You!
Jorge Chahla, M.D., Ph.D., Editorial Board, and Safa Gursoy, M.D., Ph.D.
Abstract
Articular cartilage injuries constitute a prevalent musculoskeletal problem in the general population. Restorative cartilage procedures are specifically challenging, as recapitulating hyaline cartilage can be difficult, thus compromising clinical outcomes. Progenitor cells for the treatment of articular cartilage injuries constitute a promising therapeutic method that has been increasing exponentially. Progenitor cells can be obtained from many different human tissues, such as bone marrow, adipose tissue, and muscle, as well as from peripheral blood after mobilizing stem cells from bone marrow with granulocyte colony-stimulating factor simulation. The minimally invasiveness, low complication rate, and efficacy of peripheral blood stem cells has gained significant attention and rapidly has become a promising source of progenitor cell delivery in the past decade.
Mobilized Peripheral Blood Stem Cells are Pluripotent and Can be Safely Harvested and Stored for Cartilage Repair
Arthroscopy: The Journal of Arthroscopic and Related Surgery, Article In Press. By Adam W. Anz, Johnny Torres, Hillary A. Plummer, Caroline Siew-Yoke Jee,, Travis J. Dekker, Kevin B. Johnson, and Khay-Yong Saw.
Purpose
The primary objective of this study was to reproduce and validate the harvest, processing and storage of peripheral blood stem cells for a subsequent cartilage repair trial, evaluating safety, reliability, and potential to produce viable, sterile stem cells.
Methods
Ten healthy subjects (aged 19-44 years) received 3 consecutive daily doses of filgrastim followed by an apheresis harvest of mononuclear cells on a fourth day. In a clean room, the apheresis product was prepared for cryopreservation and processed into 4 mL aliquots. Sterility and qualification testing were performed pre-processing and post-processing at multiple time points out to 2 years. Eight samples were shipped internationally to validate cell transport potential. One sample from all participants was cultured to test proliferative potential with colony forming unit (CFU) assay. Five samples, from 5 participants were tested for differentiation potential, including chondrogenic, adipogenic, osteogenic, endoderm, and ectoderm assays.
Results
Fresh aliquots contained an average of 532.9 ± 166. × 106 total viable cells/4 mL vial and 2.1 ± 1.0 × 106 CD34+ cells/4 mL vial. After processing for cryopreservation, the average cell count decreased to 331.3 ± 79. × 106 total viable cells /4 mL vial and 1.5 ± 0.7 × 106 CD34+ cells/4 mL vial CD34+ cells. Preprocessing viability averaged 99% and postprocessing 88%. Viability remained constant after cryopreservation at all subsequent time points. All sterility testing was negative. All samples showed proliferative potential, with average CFU count 301.4 ± 63.9. All samples were pluripotent.
Conclusions
Peripheral blood stem cells are pluripotent and can be safely harvested/stored with filgrastim, apheresis, clean-room processing, and cryopreservation. These cells can be stored for 2 years and shipped without loss of viability.
Level of Evidence
This method represents an accessible stem cell therapy in development to augment cartilage repair.
Massive Tibial Bone Regeneration with Autologous Peripheral Blood Stem Cells using Ilizarov Bone Transport: A Case Report
Malaysian Orthopaedic Journal 2020 Vol 14 No 3. By Saw KY, Gill R, and Low TC
ABSTRACT
This is a case report of a Gustilo-Anderson Type IIIB comminuted open right tibial fracture with massive bone loss, complicated by methicillin-resistant Staphylococus aureus (MRSA) infection. Non-viable and contaminated bony fragments were removed and infected bone resected.
Soft tissue coverage and antibiotics were effective against the MRSA infection. A unifocal bone transport with the Ilizarov method regenerated 13cm of the missing tibia. Autologous peripheral blood stem cells (PBSC) injections into the osteogenesis site boosted bone regeneration and consolidation with a shortened Bone Healing index (BHI) of 23 days/cm.
High Tibial Osteotomy in Combination With Chondrogenesis After Stem Cell Therapy : A Histologic Report of 8 Cases
Arthroscopy: The Journal of Arthroscopic and Related Surgery, Vol 31, No 10 (October), 2015: pp 1909-1920. By Khay-Yong Saw, Adam Anz, Caroline Siew-Yoke Jee, Reza Ching-Soong Ng, Norhafizah Mohtarrudin, Kunaseegaran Ragavanaidu.
Purpose
To histologically evaluate the quality of articular cartilage regeneration from the medial compartment after arthroscopic subchondral drilling followed by postoperative intra-articular injections of autologous peripheral blood stem cells (PBSCs) and hyaluronic acid with concomitant medial open-wedge high tibial osteotomy (HTO) in patients with varus deformity of the knee joint.
Methods
Eight patients with varus deformity of the knee joint underwent arthroscopic subchondral drilling of International Cartilage Repair Society (ICRS) grade 4 bone-on-bone lesions of the medial compartment with concomitant HTO. These patients were part of a larger pilot study in which 18 patients underwent the same procedure. PBSCs were harvested and cryopreserved preoperatively. At 1 week after surgery, 8 mL of PBSCs was mixed with 2 mL of hyaluronic acid and injected intra-articularly into the knee joint; this was repeated once a week for 5 consecutive weeks. Three additional intra-articular injections were administered weekly at intervals of 6, 12, and 18 months postoperatively. Informed consent was obtained at the time of hardware removal for opportunistic second-look arthroscopy and chondral biopsy. Biopsy specimens were stained with H&E, safranin O, and immunohistochemical staining for type I and II collagen. Specimens were graded using the 14 components of the ICRS Visual Assessment Scale II,and a total score was obstained.
Results
Second-look arthroscopy showed satisfactory healing of the regenerated cartilage. Histologic analysis showed significant amounts of proteoglycan and type II Collagen. The total ICRS Visual Assessment Scale II histologic scores comparing the regenerated articular cartilage (mean, 1,274) with normal articular cartilage (mean, 1,340) indicated that the repair cartilage score approached 95% of the normal articular cartilage score. There were no infections, delayed unions, or nonunions.
Conclusions
Chondrogenesis with stem cells in combination with medial open-wedge HTO for varus deformity correction of the knee joint regenerates cartilage that closely resembles the native articular cartilage.
Level of Evidence
Level IV, therapeutic case series.
Articular Cartilage Regeneration with Autologous Peripheral Blood Stem Cells Versus Hyaluronic Acid: A Randomized Controlled Trial
Arthroscopy: The Journal of Arthroscopic and Related Surgery, Vol 29, No 4 (April), 2013: pp 684-694. By Khay-Yong Saw, Adam Anz, Caroline Siew-Yoke Jee, Shahrin Merican, Reza Ching-Soong Ng, Roohi S. Ahmad, Kunaseegaran Ragavanaidu.
Purpose
The purpose of this study was to compare histologic and magnetic resonance imaging (MRI) evaluation of articular cartilage regeneration in patients with chondral lesions treated by arthroscopic subchondral drilling followed by postoperative intra-articular injections of hyaluronic acid (HA) with and without peripheral blood stem cells (PBSC).
Methods
Fifty patients aged 18 to 50 years with International Cartilage Repair Society (ICRS) grade 3 and 4 lesions of the knee joint underwent arthroscopic subchondral drilling; 25 patients each were randomized to the control (HA) and the intervention (PBSC + HA) groups. Both groups received 5 weekly injections commencing 1 week after surgery. Three additional injections of either HA or PBSC + HA were given at weekly intervals 6 months after surgery. Subjective IKDC scores and MRI scans were obtained preoperatively and postoperatively at serial visits. We performed second-look arthroscopy and biopsy at 18 months on 16 patients in each group. We graded biopsy specimens using 14 components of the International Cartilage Repair Society Visual Assessment Scale II (ICRS II) and a total score was obtained. MRI scans at 18 months were assessed with a morphologic scoring system.
Results
The total ICRS II histologic scores for the control group averaged 957 and they averaged 1,066 for the intervention group (P = .022). On evaluation of the MRI morphologic scores, the control group averaged 8.5 and the intervention group averaged 9.9 (P = .013). The mean 24-month IKDC scores for the control and intervention groups were 71.1 and 74.8, respectively (P = .844). One patient was lost to follow-up. There were no notable adverse events.
Conclusions
After arthroscopic subchondral drilling into grade 3 and 4 chondral lesions, postoperative intra-articular injections of autologous PBSC in combination with HA resulted in an improvement of the quality of articular cartilage repair over the same treatment without PBSC, as shown by histologic and MRI evaluation.
Level of Evidence
Level II, randomized controlled trial (RCT)
From Blade Runner to Stem-Cell Player and Beyond

Bone & Joint 360, Vol 2, Issue 1 (February), 2013: pp 6-11. By K-Y.Saw, C.S-Y.Jee.
Abstract
Modern athletes are constantly susceptible to performance-threatening injury as they push their bodies to greater limits and endure higher physical stresses. Loss of performance and training time can adversely and permanently affect a sportsperson’s career. Now more than ever with advancing medical technology the answer may lie in biologic therapy. We have been using peripheral blood stem cells (PBSC) clinically and have been able to demonstrate that stem cells differentiate into target cells to enable regenerative repair. The potential of this technique as a regenerative agent can be seen in three broad applications: 1) articular cartilage, 2) bone and 3) soft tissue. This article highlights the successful cases, among many, in all three of these applications.
Articular Cartilage Regeneration with Stem Cells
Modern Arthroscopy, Intech, (December), 2011, Chapter 7: pp 129-178. By Khay-Yong Saw, Adam Anz, Kathryne Stabile, Caroline SY Jee, Shahrin Merican, Yong-Guan Tay, Kunaseegaran Ragavanaidu.
Introduction
Cartilage defects continue to be a clinical challenge as regards to articular cartilage regeneration. The structure and function of articular cartilage leads to non-healing lesions after injury occurs. Well-established arthroscopic methods utilize controlled healing with marrow stimulation or transferring of non-injured cartilage to areas of injury. These include: microfracture, chondral drilling, osteochondral autograft transfer system, ostechondral allograft transplant, and autologous chondrocyte implantation. However, more often than not the treatments result in the formation of fibrocartilage and similar results within all methods with no clear superior modality (Jakobsen et al, 2005; Lubowitz et al, 2007; Magnussen et al, 2008; Nakamura et al, 2009). Recent study has investigated synthetic and biologic adjuncts to current methodology, including the use of: hyaluronic acid (HA), platelet rich plasma, mesenchymal stem cells (MSC) and peripheral blood progenitor cells (PBPC). Cell therapy has produced exciting results in animal models and has been shown to regenerate hyaline cartilage clinically in the knee joint. Our current method utilizes arthroscopic subchondral drilling of cartilage lesions in combination with a postoperative adjunct treatment involving: stimulation of the release of PBPC with filgrastim, harvest of PBPC with apheresis, and postoperative intraarticular injection of PBPC in combination with HA. Our early results lead us to the conclusion that cell therapy will have an integral part in the future treatment of cartilage damage as well as other potential orthopedic, surgical, and medical applications.
Articular Cartilage Regeneration with Autologous Peripheral Blood Progenitor Cells and Hyaluronic Acid After Arthroscopic Subchondral Drilling: A Report of 5 Cases With Histology
Arthroscopy: The Journal of Arthroscopic and Related Surgery, Vol 27, No 4 (April), 2011: pp 493-506. By Khay-Yong Saw, Adam Anz, Shahrin Merican, Yong-Guan Tay, Kunaseegaran Ragavanaidu, Caroline Jee, David A. Mcguire.
Purpose
The purpose of this study was to evaluate the quality of articular cartilage regeneration after arthroscopic subchondral drilling followed by postoperative intraarticular injections of autologous peripheral blood progenitor cells (PBPCs) in combination with hyaluronic acid (HA).
Methods
Five patients underwent second-look arthroscopy with chondral core biopsy. These 5 patients are part of a larger pilot study in which 180 patients with International Cartilage Repair Society grade III and IV lesions of the knee joint underwent arthroscopic subchondral drilling followed by postoperative intra-articular injections. Continuous passive motion was used on the operated knee 2 hours per day for 4 weeks. Partial weight bearing was observed for the first 6 to 8 weeks. Autologous PBPCs were harvested 1 week after surgery. One week after surgery, 8 mL of the harvested PBPCs in combination with 2 mL of HA was injected intra-articularly into the operated knee. The remaining PBPCs were divided into vials and cryopreserved. A total of 5 weekly intra-articular injections were given.
Results
Second-look arthroscopy confirmed articular cartilage regeneration, and histologic sections showed features of hyaline cartilage. Apart from the minimal discomfort of PBPC harvesting and localized pain associated with the intra-articular injections, there were no other notable adverse reactions.
Conclusions
Articular hyaline cartilage regeneration is possible with arthroscopic subchondral drilling followed by postoperative intraarticular injections of autologous PBPCs in combination with HA.
Level of Evidence
Level IV, therapeutic case series.
Articular Cartilage Regeneration with Autologous Marrow-Aspirate and Hyaluronic Acid: An experimental study in a goat model
Arthroscopy: The Journal of Arthroscopic and Related Surgery, Vol 25, No 12 (December), 2009: pp 1391-1400. By Khay-Yong Saw, Paisal Hussin, Seng-Cheong Loke, Mohd Azam, Hui-Cheng Chen, Yong-Guan Tay, Sharon Low, Keng-Ling Wallin & Kunaseegaran.

Purpose
The purpose of the study was to determine whether postoperative intra-articular injections of autologous marrow aspirate (MA) and hyaluronic acid (HA) after subchondral drilling resulted in better cartilage repair as assessed histologically by Gill scoring.
Methods
In a goat model we created a 4-mm full-thickness articular cartilage defect in the stifle joint (equivalent to 1.6 cm in the human knee) and conducted subchondral drilling. The animals were divided into 3 groups: group A (control), no injections; group B (HA), weekly injection of 1 mL of sodium hyaluronate for 3 weeks; and group C (HA + MA), similar to group B but with 2 mL of autologous MA in addition to HA. MA was obtained by bone marrow aspiration, centrifuged, and divided into aliquots for cryopreservation. Fifteen animals were equally divided between the groups and sacrificed 24 weeks after surgery, when the joint was harvested, examined macroscopically and histologically.
Results
Of the 15 animals, 2 from group A had died of non–surgery-related complications and 1 from group C was excluded because of a joint infection. In group A the repair constituted mainly scar tissue, whereas in group B there was less scar tissue, with small amounts of proteoglycan and type II collagen at the osteochondral junction. In contrast, repair cartilage from group C animals showed almost complete coverage of the defect with evidence of hyaline cartilage regeneration. Histology assessed by Gill scoring was significantly better in group C with 1-way analysis of variance yielding an F statistic of 10.611 with a P value of .004, which was highly significant.
Conclusions
Postoperative intra-articular injections of autologous MA in combination with HA after subchondral drilling resulted in better cartilage repair as assessed histologically by Gill scoring in a goat model.
Clinical Relevance
After arthroscopic subchondral drilling, this novel technique may result in better articular cartilage regeneration.
